UKIP deputy leader Paul Nuttall made a fool of himself on Question Time last week when he said that the NHS had two managers for every nurse. His claim has already been taken apart by Full Fact who produced this graph based on recent NHS workforce statistics.
Even if you add together all the managers and administrative staff, that’s still only 12 percent of the workforce. And if anyone wants to argue that hospital receptionists are not in frontline roles, I suggest they try being one for a day.
Of course, those of us who are familiar with crunching and analysing HR data know that raw figures rarely tell the whole story. The commentary on these statistics tells us that they are taken from the NHS’s Electronic Staff Records system. They therefore exclude temporary bank staff (many of whom are nurses), some trainee doctors and GPs and their staff, who work for separate organisations.
It’s also very difficult to pin down a number for NHS managers, as the King’s Fund said in its report in 2011.
Measuring the level of administration and management in the NHS is immensely difficult. The NHS has a plethora of statistics about managers, management
and administration, but little information that can be easily analysed about
who they are, what they do, and what their impact is. Any attempt to do that is compounded by inexact definitions that change over time.
The picture is complicated further by the number of qualified doctors and nurses in management positions or who have some management responsibility. However, the Kings Fund applied the ONS definitions of management to the NHS workforce and came to a figure of 4.8 percent. This is slightly higher than the official NHS number (just over 3 percent) but much lower than the ONS estimate of managers in the UK workforce – 15.4 percent.
In other words, the NHS has a managerial workforce a mere one-third the size of that across the economy as a whole (ONS 2010). If anything, that points to the conclusion that the NHS, particularly given the complexity of health care, is under- rather than over-managed.
The NHS in England is a £100 billion-a-year-plus business. It sees 1 million patients every 36 hours, spending nearly £2 billion a week. Aside from the banks, the only companies with a larger turnover in the FTSE 100 are the two global oil giants Shell and BP. If it were a country it would be around the thirtieth largest in the world. It might just as sensibly be asked, how can it be run effectively with only 45,000 managers.
Graeme Currie of Warwick Business School made a similar argument a couple of months ago. His research found that taking middle managers out of the NHS has led to “breaks in the information chain between day-to-day clinical practice and management structures”.
This is partly because the NHS still doesn’t properly understand and appreciate the knowledge-brokering power of what our research describes as “hybrid middle managers”. These managers may have different professional backgrounds, are located at different levels of an organisation and carry varying degrees of responsibility. What they all have in common, though, is the ability to act as a two-way mirror; capable not just of assimilating top-down management knowledge but also of translating and transmitting ideas belonging to clinical practice back up into their organisation.
In other words, the rush to take the despised middle managers out of the system may have removed some of the oil that made it run smoothly.
A study by the Chartered Management Institute published in December found that NHS investment in management development was 25 percent lower than the average across all sectors. Middle managers, it reported, were particularly missing out and showed the highest levels of disengagement among managerial staff.
I’m reminded of the comments former NHS Trust Chief Executive Lucy Moore made after joining Deloitte:
Part of the problem is that NHS doesn’t operate its leadership development at scale and never has done. It’s noticeable in my time in consulting that firms such as Deloitte invest in leadership development in a different way – operating their graduate entry as part of a much bigger leadership scheme.
The NHS Management Training Scheme is fantastic. But it is small scale, and there is nothing else really. We describe it as a National Health Service, but as far as that sort of leadership training and succession planning is concerned, it’s not at all. I’ve been very struck by that in my new life, where that is taken much more seriously.
An interesting contrast. In the commercial firm, management training is seen as an investment. There is no way a organisations like Deloitte would scrimp on training people like Lucy Moore. They are worth far too much to firm.
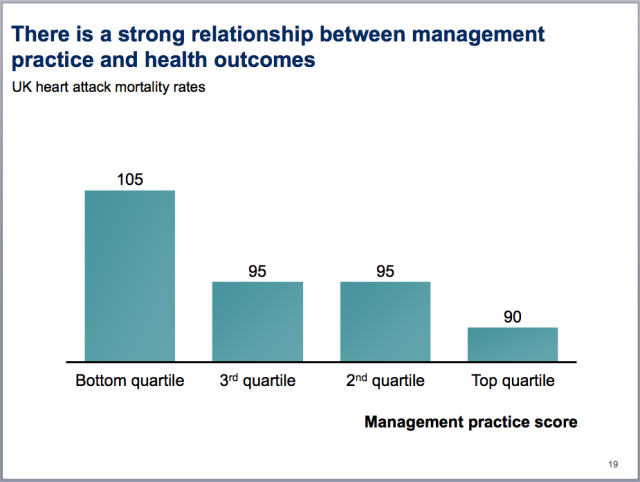
The World Management Survey (see previous post) has researched the impact of management on health systems across the world. The slide pack from August 2011 provides a good summary. (It’s worth reading to the end for the quotes.) The researchers found that doing a few simple things well, like setting objectives and managing performance, improved both clinical and financial performance.
In an earlier report, the researchers noted that, although the UK’s spending on healthcare is relatively low, its managers still performed well.
Perhaps more surprising is that when we compare these management scores against per-capita healthcare spending by country (Exhibit 6), the United Kingdom appears to deliver strong management outcomes.
 So despite low levels of investment in management, the relative performance of British healthcare managers is still pretty good. That suggests that, far from being the deadweight burden some would have us believe, NHS managers are going a lot of good things on a very tight budget.
So despite low levels of investment in management, the relative performance of British healthcare managers is still pretty good. That suggests that, far from being the deadweight burden some would have us believe, NHS managers are going a lot of good things on a very tight budget.
Under the Coalition, the number of NHS managers has been cut significantly. Some of this is due to the abolition of the Strategic Health Authorities, which, although it removes a layer of management, puts more pressure on managers elsewhere.
As if that isn’t enough, there is constant pressure to report externally. As the King’s Fund’s concluded, the NHS is under-managed but over-administered:
There is appreciable evidence that the NHS is over-administered as a result of extensive, overlapping and duplicating demands from both regulators and performance managers. There has not been a substantive review of the information demands placed on the service and its providers for many years. A review leading to a rationalisation of those demands is essential.
In other words, the targets and monitoring are coming from outside, rather than being set by local managers. The Warwick research found something similar:
First, our research has identified a real tension between patient safety knowledge that is pushed into healthcare organisations by outside stakeholders, and knowledge that is generated as a result of frontline clinical experience. Many healthcare organisations end up designing their systems around the requirement to report outwards to commissioners and regulators; yet these systems are not effective for facilitating the transfer of patient safety knowledge to and from the clinical frontline. They also mean that hybrid middle managers with designated roles for patient safety are becoming increasingly management-oriented as pressure mounts to demonstrate compliance to external bodies.
Every time there is a healthcare story in the press, another set of targets and reporting requirements appears. Recently, a committee of MPs, responding to the Stafford hospital scandal, said that hospitals should report on the number of nurses on duty each day. There’s another administrative task that will achieve…well…what, exactly?
Actually, while we’re about it, what about these headcount figures? The NHS admits they are not comprehensive. Someone should go round and add in all the missing trainees and GP staff. They should add up all the hours worked by the relief bank staff across the country and turn it into an FTE figure. Then we’d have a proper, accurate and transparent (it’s got to be transparent) figure on the true manpower level of the NHS. That would keep a few people busy for a while and tell us absolutely nothing. OK, I’m being facetious, but I wouldn’t be at all surprised if someone suggested this.
There is evidence that these constant demands for reporting on arbitrary catch-all targets are hindering, rather than helping, the running of the NHS. While managers are worrying about what the Daily Mail will make of their trust’s performance, they are spending less time doing all the useful management work that makes such a difference to the way an organisation is run.
Is the government going too far in cutting the number of NHS managers? Dr Stephen Black, of PA consulting, certainly thinks so:
The NHS target for management cost, about 0.6 to 0.8 per cent of the £70 billion GP Commissioner budget, is not only ambitious but off the scale. Only the most extraordinarily frugal charities spend less than 1 per cent on management and administration.
Highly rated charities spend 4 to 8 per cent and some well-regarded medical charities spend more than 10 per cent. The American Red Cross spends 4.5 per cent, the American Cancer Society 7 per cent, Scripps Research Institute 5 per cent and the Mayo Clinic spends more than 12 per cent.
While their activity is not entirely comparable with Britain, they still provide evidence that if central targets for management costs are imposed on the NHS, there is a risk that commissioners will be crippled before they start.
Without good managers, the NHS hasn’t a hope of making the improvements in quality and efficiency it desperately needs. Someone has to lead and co-ordinate these efforts. Cutting management to the bone will destroy the NHS’s capability to make these improvements stick. The idea that the NHS can run without good managers is just cravan populist nonsense. Every time a politician or journalist, with a poor grasp of the numbers and even less understanding of the overall picture, takes to the airwaves to rant about NHS managers, it makes the problem that bit worse.





Pingback: Is the NHS really over-managed? - Rick - Member Blogs - HR Blogs - HR Space from Personnel Today and Xpert HR
I believe the NHS is under ideological attack from neo-con members of the coalition government, led by Jeremy Hunt. They want to see an end to the NHS and it being replaced by a totally privatised healthcare service, financed solely by insurance, with extremely low level public services being provided by much-diminished very basic A&E facilities. Think America without Obamacare and a picture of what they want becomes clear.
Very interesting data.
My daughter recently had an operation on the NHS. I cannot fault the doctors and nursing staff, the care my daughter received was outstanding. However the amount of needless administration they are required to carry out is shocking.
One example was we had to sign a lengthy set of terms and conditions stating we were happy for our daughter’s name to be displayed on the wall in the nursing station (so staff could see at a glance who was in which bed, in theatre etc.) Of course we signed this but out of curiosity I asked the nurse if anyone had ever refused this permission, she laughed and said no. Given the number of operations that this one hospital ward carries out I can easily imagine this one pointless piece of paperwork taking up at least a couple of weeks per year of someone’s time to distribute, explain, collect, file and probably never refer to again.
When I hear a politician talk about efficiency savings this example is what pops into my head. Free the NHS from pointless paperwork.
It’s all tinkering at the edges.
A few managers and pen pushers culled here and there makes no difference to an organisation of the NHS’s size. The charts on staff numbers are barely statistically significant.
We will continue to gradually increase funding as a % of GDP until it eventually collapses under its own weight, or the electorate starts to realise it’s not “free” after all. Until it fails, it’s impossible to have a rational and reasoned political debate on the subject.
I do not accept that we should accept the eventual end of the NHS. This is redolent of Osborne’s current attack on social welfare standards across Europe. They are what make us civilised and the absence of which makes other parts of the world uncivilised. Less welfare means less decency and social cohesion; we should all support and defend welfare provision at all costs.
Quite so. If the NHS is struggling it is only because of political ideolism on the part of the Tories who want to eliminate all of the civil service except, presumably, themselves. As it is, even given the massively expensive and so far pointless organisational reshuffle (“Liberating the NHS” they called it – that’s a laugh!), the NHS is much cheaper to run than America’s appallingly iniquitous system, and given that every developed nation other than the USA manages to provide socialised heathcare, there seems no reason to think the NHS is unaffordable. The biggest threat faced by the NHS is the seemingly vindictive whim of the Tories, in direct contravention of their manifesto pledge.
Under managed. Over inspected. Insufficient leadership around the values that draw people to public service and health in particular. folk drawn to a vocation need leadership that will allow them flourish rather than performance management based on more or less arbitrary targets…
Change “health” to “education” in that and it describes the school system perfectly too.
As a member of the public, I can see a certain potential for miscommunication. Quoting the King’s fund quote you copied,
“There is appreciable evidence that the NHS is over-administered as a result of extensive, overlapping and duplicating demands from both regulators and performance managers.”
To me and many other people, over-administered = over managed, which then leads to more attacks on NHS managers, deserved or not. Whether or not the NHS is over managed is not necessarily correlated with the number of managers. How does it all compare with before the internal market weirdness and PFI and endless target chasing anyway?
“In other words, the rush to take the despised middle managers out of the system may have removed some of the oil that made it run smoothly.”
Reading this I was reminded of a similar management fad in the 80’s. A bit of Googling and it was referred to as the lean, mean. firm. I also see to remember that at the end of it the conclusion for a large number of companies was the same, that those middle managers played a vital role keeping the senior managers feet on the ground and translating strategy in to reality. I suspect the lesson was learnt before that as well.
On a personal note, and wary that we shouldn’t use personal experience to extrapolate to generalities, I’m undergoing some NHS care and if what I have seen compared to when I had the similar problem 5 years ago is the result of the Tory reforms then bring it on.
I understand the argument but think there is a level of semantics about management versus administration. The issue is really one of how much management/administration is productive becuase the people actually understand their area and add specific value based on tactic knowledge and experience and how much of it is “generic value” which is managerialist activity that doesn’t resolve specific issues but focuses on ticking boxes, “big pictures” and sweeping top-down programmes. Comparisons with management consultancies are interesting, because there are two strands in management consulting, the one that does specific, technocratic things like advise on technical design and implementation of complex systems where you have to know the specifics (it’s no good regurgitating PEST or SWAT when you’re being paid to implement a new server architecture), these are essentially complementing or substituting for internal middle managers with tacit knowledge (albeit at far higher cost). On the other hand there’s the “generic value” side of management consultancy that is beloved of managerialists and despised by many, which adapts and repackages generic solutions in response to specific problems at the behest of managerialists who also lack the tacit knowledge and experience to develop bottom up solutions.
It has been fashionable for a long time to complain about the number of managers in the health system; even amongst doctors and other health care staff.
If you are to be productive, you need to be able to focus on doing your job. If I, as a doctor, have to start doing administrative jobs, it distracts me from doing what I was trained to do – caring for patients. And what I want to do is doctoring, not administering or managing. So if I’m forced to do these other roles, I may not give of my best.
Managers can relieve clinicians of these tasks and, if they’re good at their jobs, can do them better. You shouldn’t really notice good management and administration. You just know that everything works as it should.
Some of the complaints have been about the rise in manager numbers. But the obvious solution – capping or reversing the number of managers – is doomed, unless the amount of management work can also be cut. Otherwise you’ll just force non-managers to do the work – probably less well, and at greater expense. Targets, the increase in regulation, inspection, and the tick-box culture that Roy Lilley (see http://snipurl.com/28gee3w for example) complains of so eloquently have vastly increased the amount of management and admin work forced onto the NHS – that’s why manager numbers have risen.
while I don’t disagree about good managers in the NHS , they are extremely hard to find. Managers in the statistics provided are those whose job titles end with director, or have clinical in the title. Junior management ranks are swelling beyond recognition.
we have nurses who are case managers, ward managers, speciality managers, every type of managers but are counted as a nurse. The measurement of a manager must be those individuals who’s hours are wholly taken up by meetings, reports and scoping exercises.
The managerial systems in th NHS are too large, too cumbersome and full of professional box tickers. Professional jealousy between groups run counter to the best solutions to the probles facing the service.
Managerial training by the NHS for the NHS will never solve the problems, simply put it is old worn out management teaching green young management the same tried and tested and failed solutions..
Innovation by staff will change the NHS but this requires encouragement rather than being managed badly by people who cannot understand the innovation.
If you keep inventing targets – as governments of both colours have been prone to do – you have to appoint managers to monitor performance against those targets.